If there was one thing Gillian knew, it was that she did not want a hole punch anywhere near her genitals.
So when, in 2018, a gynecologist recommended a vulval biopsy to check for signs of cancer, she hesitated. The doctor suspected that the whitish speck of skin that Gillian had found next to her clitoris was lichen sclerosus, a skin condition that is usually benign. To Gillian, a registered nurse, taking a chunk out of her most sensitive body part sounded a bit extreme.
But in the end she consented. He was a doctor; she was a nurse. She assumed he was the authority on this part of the body. “I never worked in OB-GYN before,” said Gillian, who asked to be identified by her first name to protect her privacy. “I was pretty clueless.”
For the biopsy, she was placed in stirrups and given a spinal epidural to numb the area. Afterward, to stem the bleeding, the doctor put one hand over the other and pressed hard against her vulva — the outer female genitalia, including the inner and outer labia, the opening to the vagina and the clitoris. Even through the anesthesia, she could feel the pressure against her pubic bone. She screamed.
A month later, Gillian was in bed with her boyfriend when she realized that she could no longer reach orgasm. She could become aroused, but at the moment of no return, “it ended into nothing,” she recalled. “And that’s still how it is.”
When she informed her gynecologist, she said, he speculated that she was experiencing numbness caused by scarring and that it would go away in time. It did not. Alarmed, Gillian began seeing one specialist after another in search of an explanation and, hopefully, a solution.
That’s when she discovered that no one wanted to talk about her clitoris.
After hearing about her injury, she said, one urologist compared her to a rape victim and said she must be having a trauma reaction to her biopsy. Next, according to her medical charts, a women’s health specialist diagnosed her with “perimenopause” and prescribed testosterone cream. Another gynecologist recommended an “O shot,” or vaginal rejuvenation procedure.
‘A side note at best’
Some urologists compare the vulva to “a small town in the Midwest,” said Dr. Irwin Goldstein, a urologist and pioneer in the field of sexual medicine. Doctors tend to pass through it, barely looking up, on their way to their destination, the cervix and uterus. That’s where the real medical action happens: ultrasounds, Pap smears, IUD insertion, childbirth.
If the vulva as a whole is an underappreciated city, the clitoris is a local roadside bar: little known, seldom considered, probably best avoided. “It’s completely ignored by pretty much everyone,” said Dr. Rachel Rubin, a urologist and sexual health specialist outside Washington, D.C. “There is no medical community that has taken ownership in the research, in the management, in the diagnosis of vulva-related conditions.”
Asked what she learned in medical school about the clitoris, Dr. Rubin replied, “Nothing that sticks out to my memory. If it got any mention, it would be a side note at best.”
Only years later, on a sexual-medicine fellowship with Dr. Goldstein, did she learn how to examine the vulva and the visible part of the clitoris, also known as the glans clitoris. The full clitoris, she learned, is a deep structure, made up largely of erectile tissue, that reaches into the pelvis and encircles the vagina.
Today, Dr. Rubin has appointed herself Washington’s premier “clitorologist.” The joke, of course, is that few are vying for the title — out of embarrassment, a lack of knowledge or fear of breaching propriety with patients. “Doctors love to focus on what we know,” she said. “And we don’t like to show weakness, that we don’t know something.”
This near-universal avoidance has consequences for patients. In a 2018 study in the journal Sexual Medicine, Dr. Rubin, Dr. Goldstein and colleagues found that a failure to examine the vulva and clitoris led doctors to regularly overlook sexual health conditions. Among women visiting Dr. Goldstein’s clinic, nearly 1 in 4 had clitoral adhesions, which occur when the hood of the clitoris sticks to the glans and can lead to irritation, pain and decreased sexual pleasure.
The authors concluded that all health providers for women should routinely examine the clitoris. But that was easier said than done, they wrote, as most providers “neither know how to examine nor feel comfortable examining the clitoris.”
This oversight has the potential to harm women, as well as trans men and other people with vulvas. There have been documented injuries to the clitoris in procedures including pelvic mesh surgeries, episiotomies during childbirth and even hip surgeries. When performed poorly, a labiaplasty — a procedure to reduce the size of the labia minora, and one of the fastest-growing cosmetic surgeries worldwide — can also damage nerves, leading to genital pain and loss of sexual sensation.
This anatomy, she stresses, isn’t magic, just biology. “It’s not just this strange, mythical area that’s supposed to give you orgasms,” she said in her office in Rockville, Md., in early July, surrounded by penile prostheses, pelvis models and a large Hitachi wand. “You should know what is what and where things are coming from.”
A tradition of neglect
So why don’t we know? To Dr. Rubin, the reason is simple: The clitoris is intimately bound up in female pleasure and orgasm. And until very recently, those themes have not been high on medicine’s priority list, nor considered appropriate areas of medical pursuit.
Gynecology, for its part, is far more focused on fertility and preventing disease. “We don’t do a great job about talking about sex from a pleasure-based perspective,” said Dr. Frances Grimstad, a gynecologist at Boston Children’s Hospital. “We talk about it from a prevention standpoint. We’re trying to prevent S.T.I.s,” or sexually transmitted infections. “We’re trying to prevent pregnancy, unless you’re trying to get pregnant. We don’t talk about sexual pleasure.”
Dr. Helen O’Connell, Australia’s first female urologist, recalled that in her own medical training, the clitoris barely made a cameo. In the 1985 edition of the medical textbook “Last’s Anatomy” that she studied, a cross-section of the female pelvis omitted the clitoris entirely, and aspects of the female genitals were described as “poorly developed” and a “failure” of male genital formation. Descriptions of the penis went on for pages. To her, this widespread medical disregard helped explain why her urology peers worked to preserve nerves in the penis during prostate surgeries but not during pelvic surgeries on women.
Dr. O’Connell set out to investigate the full anatomy of the clitoris using microdissection and magnetic resonance imaging. In 2005, she published a comprehensive study showing that the outer nub of the clitoris — the part that can be seen and touched — was just the tip of the iceberg, equivalent to the head of the penis. The full organ extended far beneath the surface, comprising two teardrop-shaped bulbs, two arms and a shaft.
By failing to appreciate this anatomy, she warned, surgeons working in this region risked damaging the sensitive nerves responsible for pleasure and orgasm, which run along the top of the shaft. In procedures like pelvic mesh surgeries or urethral surgeries, “things are potentially in the crossfire,” Dr. O’Connell said. “You always need to be thinking of what’s underneath, what’s hidden from view that you’re potentially altering.”
Increasingly, women are speaking out about injuries they sustained to this area during routine procedures. One is Julie, a 44-year-old office manager in Essex, east of London, who lost her ability to orgasm in 2012 after a minimally invasive hip operation to address back pain. She shared her story publicly in The Telegraph last year, using only her first name to avoid discrimination by future employers.
During a Zoom call in January, Julie described waking up from anesthesia to a searing pain around her clitoris. Her surgeon told her that it was just bruising and would fade. A few months later, she found that she could no longer orgasm. When she tried, “it was literally like someone had pulled a plug out of the socket,” she said. “Everything went dead.”
It took two years of internet searching for her to realize that a cylindrical post placed between her legs during the operation had likely crushed her clitoral nerves. Use of the device, called a perineal post, is known to cause nerve damage, but this was not mentioned on her consent form.
Julie compared her injury to losing the sense of taste or smell — a pleasure taken for granted but when lost changes everything. “It’s 10 years, and I still can’t believe it,” she said over Zoom. “And I haven’t come to terms with it.”
Gillian is still trying to understand the cause of her own injury. Was it the biopsy? The crushing pressure her gynecologist applied afterward? Four years and 12 specialists later, she has resigned herself to the fact that she may never recover that sensation. “This changed my whole life,” she said. “The devastation from this is something you can never repair. Ever.”
A new medical map
When Dr. Blair Peters, a 33-year-old plastic surgeon at Oregon Health & Science University, first began performing phalloplasties for trans men and nonbinary people, he was surprised to see how large the nerves of the clitoris were — about three millimeters in diameter, on average. (By comparison, the sensory nerve of the index finger is about one millimeter wide.)
“When I went through medical school, we did not learn anything in particular about the clitoris beyond the fact that it exists, basically,” said Dr. Peters. As a result, he said, he developed “this subconscious bias that it’s not going to be this superapparent structure. But it is.”
Dr. Peters is among a handful of young, social media-savvy doctors who, like Dr. Rubin, are helping expand medicine’s map of this terrain — and, in doing so, ensure that what happened to Julie and Gillian doesn’t happen again. As part of his efforts to improve sexual sensation for phalloplasty patients, Dr. Peters recently magnified clitoral nerves and counted up how many nerve fibers they contained. The number he found — embargoed until he presents his findings at a conference later this month — was “significantly more” than 8,000, the figure often cited, which is drawn from an outdated study on cows.
In 2020, Victoria Gordon, a medical student at the Kansas City University of Medicine and Biosciences, led a study that sought to define a “danger zone” around the clitoris for plastic surgeons to avoid. During dissections of cadavers, she noticed that clitoral nerves sometimes branch out into fine tendrils, like roots, in ways that might be relevant to surgeons but were not previously described in the literature.
She hoped that others in the plastic surgery field would follow up on this finding, which was published in a plastic surgery journal. “I’m just a fourth-year medical student, I don’t think I should have to tackle this project,” she said in late 2021. “But no one else is.”
Doctors are not the only people urging medicine to recognize the full anatomy of the clitoris. In 2018, Gillian was searching online to make sense of her injury when she came across a Medium post by a woman in Dallas, Jessica Pin, whose situation sounded eerily like hers. Ms. Pin, now 36, had lost most of her clitoral sensation after undergoing a labiaplasty at age 18.
After scouring the major obstetrical-gynecologicial textbooks, Ms. Pin learned that the nerves of the clitoris were rarely well represented, if at all — a key oversight that she believed left the clitoris at risk in a number of procedures. “This omission appears to be caused by sociocultural discomfort with the clitoris and a pervasive lack of regard for female sexual response,” she wrote on Medium.
Gillian was intrigued. “She was the only one talking about this on the internet,” she said. She sent the woman a Facebook message.
Ms. Pin eventually began a social media campaign to get OB-GYN textbooks and training standards updated to cover this anatomy. Gillian quietly helped her build followers, then joined Ms. Pin on Instagram, using the handle @nursevulvaadvocate. There, she found herself fielding hundreds of queries from around the world from people who had lost genital sensation as a result of medical procedures on or near the clitoris.
Gillian tried to respond to everyone, she said, but could not offer the medical advice that many of them sought. After six months, she closed her account. Today her efforts are more local: She often drives to doctors’ offices to drop off posters of clitoral anatomy. In her work with older patients, she pays close attention to any genital concerns, from vulvar itching to pain after cancer surgery.
Yet her tactics are not without controversy. She has been embroiled in numerous social media disputes, and has been accused of harassment for her persistent and sometimes inappropriate efforts to reach gynecologists and anatomy textbook authors.
Now, after four years of advocating, “I want to be done,” she said. “It would be amazing if doctors start picking up the cause and start talking about this.” The fact that a few medical professionals have, including Dr. Rubin, is “a really big deal,” she added.
Giving the vulva its due
Every patient who enters Dr. Rubin’s office, regardless of age, is taken on a tour of their own vulva. No longer is a sheet draped over a patient’s legs for the pelvic exam — a convention that Dr. Rubin believes helps keep women’s “private parts” shameful and hidden. Instead, Dr. Rubin starts by handing her patient a long-handled mirror to see the same anatomy that she will be examining.
With a Q-tip, Dr. Rubin probes each part of the vulva for pain, pointing out the labia minora, labia majora and vaginal opening as her patient follows along. Then, she checks under the clitoral hood for adhesions or other skin conditions. The entire exam usually takes under five minutes. “We go at your pace,” she said recently in an exam with a 62-year-old woman, who was experiencing pain after sex. “You’re the boss of this show.”
Dr. Rubin and her colleagues believe that their field is uniquely positioned to champion the clitoris and female pleasure. After all, said Dr. Barbara Chubak, a urologist at the Icahn School of Medicine at Mount Sinai hospital in New York, “urologists are all about the phallus” — which the clitoris technically is, as it arises from the same embryological structures and is made up of the same erectile tissues as the penis.
“So by definition, clitoral anatomy could, and should, also be a urologic thing,” Dr. Rubin added.
Moreover, urologists are perfectly comfortable waxing poetic about things that other providers are too squeamish to discuss. “Urology is all about peeing and all about sex,” Dr. Chubak said. “The stuff that people are embarrassed to talk about, urologists want to talk about. Clitoral medicine belongs with the urologists.”
Still, it will take more than passionate “penis doctors,” Dr. Rubin said, to give the vulva its due; there must be a concerted movement, one that transcends medicine’s traditionally siloed specialties, to understand and map this anatomy. And for that to happen, other fields need to recognize female sexual pleasure as essential and worth preserving.
“I truly believe we are just several decades behind on the female side,” Dr. Rubin said. “But we have to do the work. And we have to have people interested in doing the work.”
Rachel E. Gross is the author of “Vagina Obscura: An Anatomical Voyage.”
There is
a lot scientists still don’t know about the female reproductive system. They
don’t know enough about how to treat the most common vaginal infection,
bacterial vaginosis. They don’t have good solutions for many people suffering
from endometriosis, a common and sometimes incredibly painful condition where
tissue similar to what grows inside the uterus grows elsewhere in the body.
They still have a lot of questions about what menopause does to a body.
So a few years ago, Rachel Gross, a science reporter who focuses on reproductive health, set out to write a book about the mysteries of the female reproductive system. But as she dove into the research, she started to wonder about the phrase she was using — the phrase “female reproductive system.”
First, not everyone with the organs she was researching was female. She was speaking to nonbinary people, intersex people, trans people; all people for whom this anatomy was relevant and intimate.
Also, the idea that these organs — the clitoris, the vagina, even the ovaries — were only playing a role in reproduction started to feel reductive. Of course, these organs are involved in baby-making, but, she says, “I was finding that they were doing so much else, not just sexual stuff, which is huge and often overlooked, but they were participating in immunity and protection and regeneration.”
On Unexplainable — Vox’s podcast that explores big mysteries, unanswered questions, and all the things we learn by diving into the unknown — Gross talks about one of these organs: the ovaries. She tells us a familiar story: that the ovaries are “biological clocks” that only lose eggs, without ever gaining any back. But then, she walks us through new research that questions that idea, suggesting that the ovaries may be able to generate new eggs using stem cells.
And, as Gross explains, this new way of understanding and imagining the ovaries might lead to new fertility treatments — but also, potentially, new ways to treat some of the health effects associated with menopause, like loss of bone density.
In her book, Vagina Obscura: An Anatomical Voyage, Gross finds many examples of metaphors like the ovarian “ticking clock,” or even whole stories about various pelvic organs, that have stymied science and maybe even kept scientists from solving some of the big questions about these organs.
“When you study the human body, even though the human body is not changing, you really see what you expect to see … and you kind of just blur out the rest,” she says.
I asked Gross to walk me through some more examples from her book. What follows is our conversation, edited for clarity and length.
Byrd Pinkerton:
What’s an example of an organ we’ve told an incorrect story about and how it misguided science?
Rachel Gross:
So one big example is the clitoris. It has been called a minuscule phallus or an underdeveloped penis or a tiny nub for hundreds and hundreds of years. And science has sort of minimized it in many ways, from literally omitting it in anatomical textbooks to just not studying 90 percent of it, which is under the surface.
It took a female urologist to say, “Wait, the research on the female side is a lot less rigorous than the male side. We haven’t looked at all the nerves, the erectile bodies.”
She found out that the clitoris has these roots and these bulbs that actually hug the vagina and swell with blood and become erectile just like the penis. So you have the exact same erectile tissues, you have the head — or the glans clitoris — which is the part you can see and touch. But then you also have a shaft that goes back into the body and you have bulbs and kind of arms that flow back into the pelvis. And all of these are made up with the same erectile tissues as the penis.
These things are super important for women undergoing surgery in this area who don’t want their nerves cut off.
If you look at it [the clitoris] as a homologous organ [to the penis], you come to such a different conclusion than it’s a tiny phallus or a little nub that’s hard to find.
Byrd Pinkerton:
[At the beginning of her book, Rachel Gross describes a personal experience. She got a persistent vaginal infection, and her gynecologist recommended that she put boric acid in her vagina. The poison would kill a lot of the organisms in her vagina, including, hopefully, the one causing her problems.
Boric acid is also used as a rat poison, however, so the harshness of the treatment surprised Gross. And as she dived into the research, she realized that a new way of imagining the vagina might lead to more effective, less poisonous treatments.]
You talked about putting this boric acid pill into your vagina. Is that treatment based on any outdated story or a metaphor around the vagina that people are reconsidering?
Rachel Gross:
So I think there’s been a strong attitude toward the vagina of like ... it should be pure, it should be clean, it should be sterile. And from that you get all of these vaginal cleansing products. What blew my mind was looking at the vaginal microbiome as this teeming ecosystem of protection instead.
Byrd Pinkerton:
What is the vaginal microbiome?
Rachel Gross:
So, you’ve heard of the gut microbiome, the specific bacteria that help maintain digestive health.
Byrd Pinkerton:
Yep.
Rachel Gross:
Well, your vagina also has a microbiome, and it’s actually really unique to humans. It’s a mildly acidic environment created by mostly bacteria called lactobacilli, but also other bacteria, some viruses, and fungi. And they all live in harmony and protect you from invaders and kind of keep this liminal space between you and not-you healthy. It’s up against whatever gets up there, whether that is tampons, semen, birth control, jade eggs, other stuff you put in there ... like your vagina is responding, protecting you and reaching a new equilibrium.
Byrd Pinkerton:
Interesting. So if you’re thinking of that space as like a garden that fends off invaders, it does feel like you would reimagine putting rat poison in the middle of your garden.
Rachel Gross:
Exactly. If you reimagine it as a garden and it’s fine to have weeds and different species in a garden, then it’s not about stripping it of life, which is what the rat poison does. It’s about cultivating the right mix. And that has led to innovations in vaginal microbiome transplants or probiotics that could kind of terraform the vagina. All these different ideas, it’s not clear that all of them will work, but there’s just so many smarter and more imaginative ways to think of having a healthy vagina.
Byrd Pinkerton:
So, do we know anything about our bodies? Or is it all just sort of stories we’re telling ourselves that are shaping the directions that we’re taking?
Rachel Gross:
I do think that we know a lot about bodies and we use that knowledge very practically in medicine to heal them and make things better. But there’s a lens of language that just directs the questions we’re asking and what we consider interesting and worthwhile. So could you swing that lens a little to the left, to the part that’s all blurred out, and focus on that? And what would you see?
Byrd Pinkerton:
How do you swing the lens and reshape what we know about the reproductive system?
Rachel Gross:
By introducing new people with new backgrounds into science and having them ask their questions and be interested in what they’re interested in. And for a long time, we’ve had a very similar lens.
You had people that were centering the male body as representing something and looking at the female body as an afterthought or as something that was mainly involved in reproduction. That’s mainly the interesting difference between types of bodies. So yeah, my whole book is about how once you get new voices and people in science, the whole lens changes in really exciting ways.
The ovarian “biological clock” and other reproductive health metaphors that have led science astray. By Byrd Pinkerton. Vox, August 17, 2022.
So a few years ago, Rachel Gross, a science reporter who focuses on reproductive health, set out to write a book about the mysteries of the female reproductive system. But as she dove into the research, she started to wonder about the phrase she was using — the phrase “female reproductive system.”
First, not everyone with the organs she was researching was female. She was speaking to nonbinary people, intersex people, trans people; all people for whom this anatomy was relevant and intimate.
Also, the idea that these organs — the clitoris, the vagina, even the ovaries — were only playing a role in reproduction started to feel reductive. Of course, these organs are involved in baby-making, but, she says, “I was finding that they were doing so much else, not just sexual stuff, which is huge and often overlooked, but they were participating in immunity and protection and regeneration.”
On Unexplainable — Vox’s podcast that explores big mysteries, unanswered questions, and all the things we learn by diving into the unknown — Gross talks about one of these organs: the ovaries. She tells us a familiar story: that the ovaries are “biological clocks” that only lose eggs, without ever gaining any back. But then, she walks us through new research that questions that idea, suggesting that the ovaries may be able to generate new eggs using stem cells.
And, as Gross explains, this new way of understanding and imagining the ovaries might lead to new fertility treatments — but also, potentially, new ways to treat some of the health effects associated with menopause, like loss of bone density.
In her book, Vagina Obscura: An Anatomical Voyage, Gross finds many examples of metaphors like the ovarian “ticking clock,” or even whole stories about various pelvic organs, that have stymied science and maybe even kept scientists from solving some of the big questions about these organs.
“When you study the human body, even though the human body is not changing, you really see what you expect to see … and you kind of just blur out the rest,” she says.
I asked Gross to walk me through some more examples from her book. What follows is our conversation, edited for clarity and length.
Byrd Pinkerton:
What’s an example of an organ we’ve told an incorrect story about and how it misguided science?
Rachel Gross:
So one big example is the clitoris. It has been called a minuscule phallus or an underdeveloped penis or a tiny nub for hundreds and hundreds of years. And science has sort of minimized it in many ways, from literally omitting it in anatomical textbooks to just not studying 90 percent of it, which is under the surface.
It took a female urologist to say, “Wait, the research on the female side is a lot less rigorous than the male side. We haven’t looked at all the nerves, the erectile bodies.”
She found out that the clitoris has these roots and these bulbs that actually hug the vagina and swell with blood and become erectile just like the penis. So you have the exact same erectile tissues, you have the head — or the glans clitoris — which is the part you can see and touch. But then you also have a shaft that goes back into the body and you have bulbs and kind of arms that flow back into the pelvis. And all of these are made up with the same erectile tissues as the penis.
These things are super important for women undergoing surgery in this area who don’t want their nerves cut off.
If you look at it [the clitoris] as a homologous organ [to the penis], you come to such a different conclusion than it’s a tiny phallus or a little nub that’s hard to find.
Byrd Pinkerton:
[At the beginning of her book, Rachel Gross describes a personal experience. She got a persistent vaginal infection, and her gynecologist recommended that she put boric acid in her vagina. The poison would kill a lot of the organisms in her vagina, including, hopefully, the one causing her problems.
Boric acid is also used as a rat poison, however, so the harshness of the treatment surprised Gross. And as she dived into the research, she realized that a new way of imagining the vagina might lead to more effective, less poisonous treatments.]
You talked about putting this boric acid pill into your vagina. Is that treatment based on any outdated story or a metaphor around the vagina that people are reconsidering?
Rachel Gross:
So I think there’s been a strong attitude toward the vagina of like ... it should be pure, it should be clean, it should be sterile. And from that you get all of these vaginal cleansing products. What blew my mind was looking at the vaginal microbiome as this teeming ecosystem of protection instead.
Byrd Pinkerton:
What is the vaginal microbiome?
Rachel Gross:
So, you’ve heard of the gut microbiome, the specific bacteria that help maintain digestive health.
Byrd Pinkerton:
Yep.
Rachel Gross:
Well, your vagina also has a microbiome, and it’s actually really unique to humans. It’s a mildly acidic environment created by mostly bacteria called lactobacilli, but also other bacteria, some viruses, and fungi. And they all live in harmony and protect you from invaders and kind of keep this liminal space between you and not-you healthy. It’s up against whatever gets up there, whether that is tampons, semen, birth control, jade eggs, other stuff you put in there ... like your vagina is responding, protecting you and reaching a new equilibrium.
Byrd Pinkerton:
Interesting. So if you’re thinking of that space as like a garden that fends off invaders, it does feel like you would reimagine putting rat poison in the middle of your garden.
Rachel Gross:
Exactly. If you reimagine it as a garden and it’s fine to have weeds and different species in a garden, then it’s not about stripping it of life, which is what the rat poison does. It’s about cultivating the right mix. And that has led to innovations in vaginal microbiome transplants or probiotics that could kind of terraform the vagina. All these different ideas, it’s not clear that all of them will work, but there’s just so many smarter and more imaginative ways to think of having a healthy vagina.
Byrd Pinkerton:
So, do we know anything about our bodies? Or is it all just sort of stories we’re telling ourselves that are shaping the directions that we’re taking?
Rachel Gross:
I do think that we know a lot about bodies and we use that knowledge very practically in medicine to heal them and make things better. But there’s a lens of language that just directs the questions we’re asking and what we consider interesting and worthwhile. So could you swing that lens a little to the left, to the part that’s all blurred out, and focus on that? And what would you see?
Byrd Pinkerton:
How do you swing the lens and reshape what we know about the reproductive system?
Rachel Gross:
By introducing new people with new backgrounds into science and having them ask their questions and be interested in what they’re interested in. And for a long time, we’ve had a very similar lens.
You had people that were centering the male body as representing something and looking at the female body as an afterthought or as something that was mainly involved in reproduction. That’s mainly the interesting difference between types of bodies. So yeah, my whole book is about how once you get new voices and people in science, the whole lens changes in really exciting ways.
The ovarian “biological clock” and other reproductive health metaphors that have led science astray. By Byrd Pinkerton. Vox, August 17, 2022.
In the
17th century, ovaries got their modern name, which essentially means “place for
eggs”. Before that, they were known only as female testicles, thought to be
vestigial versions of male gonads that may or may not produce “female sperm”. A
young Dutch anatomist, Regnier de Graaf, was the first to show that they
actually made eggs, by dissecting just-mated rabbits. “Nature had her mind on
the job when generating the female as well as when generating the male,” he
wrote.
But in the 19th century, the trend of surgeons removing healthy ovaries to treat “ailments” such as hysteria made it clear that they were doing far more than acting as egg baskets. These unassuming organs were, in fact, supporting women’s wellbeing in a much more fundamental way. Eventually, the discovery of estrogen helped scientists piece together the fact that the ovaries were powerhouses of female health, nodes in a complex feedback mechanism between brain and body. They orchestrated the production of hormones that supported nearly every physical system, from bones to brain development.
The “egg basket” concept is typical of the way that, for centuries, scientists have viewed women primarily in one dimension: as baby-makers. And yet, even when it comes to the organs that participate directly in reproduction, this can lead to bad science and missed opportunities.
But in the 19th century, the trend of surgeons removing healthy ovaries to treat “ailments” such as hysteria made it clear that they were doing far more than acting as egg baskets. These unassuming organs were, in fact, supporting women’s wellbeing in a much more fundamental way. Eventually, the discovery of estrogen helped scientists piece together the fact that the ovaries were powerhouses of female health, nodes in a complex feedback mechanism between brain and body. They orchestrated the production of hormones that supported nearly every physical system, from bones to brain development.
The “egg basket” concept is typical of the way that, for centuries, scientists have viewed women primarily in one dimension: as baby-makers. And yet, even when it comes to the organs that participate directly in reproduction, this can lead to bad science and missed opportunities.
For example, menopause is often described as the end of a woman’s “reproductive years” and the point at which her ovaries “fail” or “exhaust” themselves. In fact, we now know that ovaries continue to make crucial hormones even after that transition. And, astonishingly, scientists have identified ovarian stem cells with the potential to grow into new eggs, including in postmenopausal women. This raises the prospect of new treatments for infertility or hormonal disorders, and calls into question just how much we actually know about the mechanisms behind menopause.
The roots of this reproductive bias go back thousands of years. In ancient Greece, women were believed to be controlled by their unruly wombs – with the unruliness often caused by a failure to bear children in a timely manner. If she stayed unmarried too long after puberty, it was thought, a woman’s uterus would trample around her body like a bratty toddler, causing all manner of unpleasant symptoms. That idea would ultimately evolve into the notion of hysteria, with its roots in the Greek word for womb, hystera.
This deeply ingrained prejudice once again led to gaps in our knowledge, and a great deal of suffering. Consider endometriosis, a condition that arises when tissue similar to the lining of the womb grows in other places around the body. Medical textbooks as late as the 1990s deemed it “the career woman’s disease”, describing it as afflicting women who had foregone marriage and children to pursue their professional lives. Some doctors even suggested pregnancy as a “cure” (and still do today, despite the fact that the idea has long been disproved).
This kind of thinking has stymied our understanding of an incredibly common, painful disease – one that affects women who have already given birth, girls before their periods as well as trans men and nonbinary people. Today, researchers are finally beginning to see endometriosis for what it really is: a body-wide chronic inflammatory disease. That new understanding is opening the door to potential treatments that don’t rely on manipulating hormone levels or shutting down the menstrual cycle altogether.
Centring reproduction has also sidelined body parts that, while nominally considered part of “the reproductive system,” are really more about sex and pleasure. Specifically, the clitoris, which was once famously dismissed by the father of modern anatomy, Andreas Vesalius, as “this new and useless part”. In his eyes, the female body was an inversion of the male’s: the uterus was an inside-out penis, and the ovaries were interior testicles. According to that framework, women already had all the body parts they needed, no clitoris required.
It is no coincidence that the clitoris would continue to be lost and rediscovered by men of science throughout anatomical history. In the 1990s, it was often omitted or minimised in medical textbooks, with diagrams pointing to the glans clitoris – equivalent to the head of the penis – as the entire thing. Even today, this organ is glossed over in medical training, its role in healthy sexual function, and therefore human health in general, downplayed. The resulting lack of understanding can lead to clitoral injury for women who go under the knife for things such as pelvic mesh removal, urethral procedures, vulval biopsies, and even hip surgeries. Because gynaecologists rarely examine the clitoris, problems such as clitoral adhesions or cancers of the vulva may also be missed or diagnosed late.
In some ways, the consequences of all this skewed science down the ages are obvious: we now face a huge knowledge gap when it comes to half the bodies on Earth. The fact that science still doesn’t know exactly how these important organs work when they aren’t contributing to making a baby is disturbing, to say the least.
But the effects are broader than that. Female health is not its own planet, divorced from male health. We all share the same universal body plan, the same origins in the womb, the same hormones and basic bodily processes. Therefore, almost all of these issues have parallels in male bodies. Researchers who study endometriosis, for example, find that patterns of inflammation that underlie this disease also affect male health. Research into the vaginal microbiome sheds light on the penile microbiome. Studying menstruation teaches us about universal biological processes such as regeneration and scarless wound healing.
For centuries, science has been treating women as walking wombs, baby machines and incubators of new life. This narrow perspective has prevented us from asking questions and making advancements that could help all of us live longer, healthier lives. It’s time for a paradigm shift. We need to finally see the female body for what it truly is: a powerful constellation of interlocking elements, each part indivisible from the whole, that work together to support our health from cradle to grave. As we fill in the missing parts of this picture, we will undoubtedly expand our understanding of all bodies.
Rachel E Gross is the author of Vagina Obscura: An Anatomical Voyage (WW Norton).
The big idea: why we need to rewrite the history of female bodies. By Rachel E. Gross. The Guardian, May 9, 2022.
“There
comes a time in every woman’s life when she sees herself as medicine has seen
her: a mystery. An enigma. A black box that, for some reason, no one has
managed to get inside.”
—Rachel E. Gross
Ten years ago, I went to see my ob-gyn, complaining of pain with sex. A pelvic examination revealed nothing. “Everything looks okay down there,” she said from her three-legged stool, adding that she would order a pelvic ultrasound. She paused a moment, then uttered words that would haunt me.
“Pelvic pain is the black box of gynecology.”
A decade on, no one has completely cracked the black box of my pain. At least now I have a diagnosis: pudendal neuralgia (PN), or chronic pain of a pelvic nerve, brought on by long-distance cycling. It took months, and a trip to a knowledgeable physical therapist, to learn I had PN. My ob-gyn’s words were prophetic. She couldn’t figure out what was wrong with me, and while I finally found a doctor who helped relieve my symptoms, he retired at the end of 2018, and I’ve struggled with pain flares ever since.
Rachel E. Gross opens her debut book Vagina Obscura: An Anatomical Voyage with a vaginal complaint that, like mine, eluded gynecological knowledge. Back in 2018, she was diagnosed with an infection that persisted through one antifungal treatment and two rounds of antibiotics. Finally, her doctor prescribed a treatment that was “basically rat poison” (these were her doctor’s actual words). Gross dutifully inserted the medication vaginally until, in a middle-of-the-night stupor, she unthinkingly swallowed a suppository and ended up in the ER.
Like me, Gross had stumbled into what she calls a “black box” moment. “There comes a time in every woman’s life,” Gross writes, when “she sees herself as medicine has seen her: a mystery. An enigma. A black box that, for some reason, no one has managed to get inside.”
Luckily, as an online science editor for Smithsonian Magazine, Gross was poised to, if not crack every secret, certainly explore female anatomy’s many “mysteries.” Across eight chapters with titles like, “Desire (Glans Clitoris),” “Power (Ovaries)” and “Beauty (Neovagina),” Gross takes us on a journey around the female body, elaborating both on what science knows, and what it doesn’t: It wasn’t until 1993 that a federal mandate required researchers to include women and minorities in clinical research.
Gross recently spoke to me by phone from her home in Brooklyn. Thoughtful and erudite, she talked about the female and LGBT researchers who’ve made scientific inroads against the odds, the myth that the “clitoral” and “vaginal” orgasms are distinct from each other, a princess who relocated her clitoris, koala vaginas and much more.
Carli Cutchin: Let’s talk about why you wrote Vagina Obscura. What gaps in awareness and knowledge did you see, and how does the book address them?
Rachel Gross: The introduction maybe gave the impression my own vaginal infection was the impetus. It was more of a crystalizing moment. At that point, I’d been the online science editor at Smithsonian Magazine for two years. I’d expanded their coverage of women in science and, separately, reproductive biology. We would do stories like the history of the modern IUD and how medical schools are developing a “robotic” vagina for medical training. Then I helped launch this column on unsung women in science—how they transformed their fields and the systemic hurdles they faced.
I started realizing there was an intersection between these two types of coverage. For a long time, women and LGBT scientists had been marginalized. They hadn’t been the ones asking questions. This marginalization of women and other gender minorities from science, I began to see, was closely tied to the marginalization of women’s bodies from science. I wanted to spotlight the factors leading to why these particular areas of the human body were misunderstood and understudied. [Vagina Obscura] tries to chronicle the people who did ask these groundbreaking questions, and the challenges they faced.
Cutchin: The first chapter, “Desire (Glans Clitoris)” tells of Marie Bonaparte, who went to great lengths to achieve a “vaginal orgasm,” which Sigmund Freud had recently deemed the pinnacle of properly feminine pleasure—though, unlike Freud, Marie believed anatomy and not psychology was keeping her from vaginal climax. What drew you to Marie’s story?
—Rachel E. Gross
Ten years ago, I went to see my ob-gyn, complaining of pain with sex. A pelvic examination revealed nothing. “Everything looks okay down there,” she said from her three-legged stool, adding that she would order a pelvic ultrasound. She paused a moment, then uttered words that would haunt me.
“Pelvic pain is the black box of gynecology.”
A decade on, no one has completely cracked the black box of my pain. At least now I have a diagnosis: pudendal neuralgia (PN), or chronic pain of a pelvic nerve, brought on by long-distance cycling. It took months, and a trip to a knowledgeable physical therapist, to learn I had PN. My ob-gyn’s words were prophetic. She couldn’t figure out what was wrong with me, and while I finally found a doctor who helped relieve my symptoms, he retired at the end of 2018, and I’ve struggled with pain flares ever since.
Rachel E. Gross opens her debut book Vagina Obscura: An Anatomical Voyage with a vaginal complaint that, like mine, eluded gynecological knowledge. Back in 2018, she was diagnosed with an infection that persisted through one antifungal treatment and two rounds of antibiotics. Finally, her doctor prescribed a treatment that was “basically rat poison” (these were her doctor’s actual words). Gross dutifully inserted the medication vaginally until, in a middle-of-the-night stupor, she unthinkingly swallowed a suppository and ended up in the ER.
Like me, Gross had stumbled into what she calls a “black box” moment. “There comes a time in every woman’s life,” Gross writes, when “she sees herself as medicine has seen her: a mystery. An enigma. A black box that, for some reason, no one has managed to get inside.”
Luckily, as an online science editor for Smithsonian Magazine, Gross was poised to, if not crack every secret, certainly explore female anatomy’s many “mysteries.” Across eight chapters with titles like, “Desire (Glans Clitoris),” “Power (Ovaries)” and “Beauty (Neovagina),” Gross takes us on a journey around the female body, elaborating both on what science knows, and what it doesn’t: It wasn’t until 1993 that a federal mandate required researchers to include women and minorities in clinical research.
Gross recently spoke to me by phone from her home in Brooklyn. Thoughtful and erudite, she talked about the female and LGBT researchers who’ve made scientific inroads against the odds, the myth that the “clitoral” and “vaginal” orgasms are distinct from each other, a princess who relocated her clitoris, koala vaginas and much more.
Carli Cutchin: Let’s talk about why you wrote Vagina Obscura. What gaps in awareness and knowledge did you see, and how does the book address them?
Rachel Gross: The introduction maybe gave the impression my own vaginal infection was the impetus. It was more of a crystalizing moment. At that point, I’d been the online science editor at Smithsonian Magazine for two years. I’d expanded their coverage of women in science and, separately, reproductive biology. We would do stories like the history of the modern IUD and how medical schools are developing a “robotic” vagina for medical training. Then I helped launch this column on unsung women in science—how they transformed their fields and the systemic hurdles they faced.
I started realizing there was an intersection between these two types of coverage. For a long time, women and LGBT scientists had been marginalized. They hadn’t been the ones asking questions. This marginalization of women and other gender minorities from science, I began to see, was closely tied to the marginalization of women’s bodies from science. I wanted to spotlight the factors leading to why these particular areas of the human body were misunderstood and understudied. [Vagina Obscura] tries to chronicle the people who did ask these groundbreaking questions, and the challenges they faced.
Cutchin: The first chapter, “Desire (Glans Clitoris)” tells of Marie Bonaparte, who went to great lengths to achieve a “vaginal orgasm,” which Sigmund Freud had recently deemed the pinnacle of properly feminine pleasure—though, unlike Freud, Marie believed anatomy and not psychology was keeping her from vaginal climax. What drew you to Marie’s story?
Gross: Marie Bonaparte is a figure with such a particular lens. She’s a noblewoman, the great-grandniece of Napoleon. She grows up in interwar France and really wants to be a doctor but is thwarted in that ambition because she has to “marry rich” and do what’s expected of her station. She ends up becoming besties with Freud—becoming his pupil, challenging him on some of his core beliefs about female sexuality, then personally acting on [her] theories. She develops an experimental surgery to literally relocate her clitoris so she could experience what Freud had deemed the “vaginal orgasm.”
[Spoiler alert: The surgery didn’t produce the desired results.]
She’s such a complex woman who clearly had original ideas, is fearless about pursuing them in both her personal and professional life and surmounts a lot of obstacles to do medical research and get it published in peer-reviewed journals under a male surname. At the same time, she’s an incredibly privileged woman who has access to resources that few people could dream of: to Freud himself, to ob-gyn offices, and to women she ends up interviewing across the world.
She also has some very problematic ideas about race—[ideas] that she’s not alone in having in her time, but are limited and backward. She’s one of these complex figures from history. Her story is worth telling because it shows how Freud’s theories trickled down to women’s actual relationship with their bodies, but she was also someone I wanted to be careful not to heroize. And this is the case with most of these historical figures, including women scientists. They are going to be fascinating and flawed and often contradictory.
Cutchin: In fact, Marie Bonaparte and Freud were wrong about the female orgasm, as you relate in Chapter 2. There’s really no distinction between clitoral and vaginal orgasms, because, as Helen O’Connell, a groundbreaking Australian urologist, points out, the clitoris is not a single organ but a “cluster of erectile tissues” that hug the vagina and urethra. During vaginal penetration, sensation actually comes from the stimulation of the clitoris through vaginal walls.
I have to say I was stunned when I read this, and I’ve been telling anyone who will listen about it ever since. How might this information change the way people with vaginas approach sexuality and pleasure?
Gross: I hesitate to give advice; I’m not a sex therapist. I would in hope in some ways it doesn’t change what people are doing, which is hopefully exploring their bodies with curiosity, finding what works for them in terms of sexuality and pleasure and orgasm.
What I took away from that research was that our conception of our own bodies—those of us who identify as women—could look very different. I found that from the Greeks to Freud, there’s been this strong tendency to divide up female genitals into separate parts.
There’s this pattern where people are always trying to say, “Oh, these bulbs? They’re not part of the clitoris. We’ll just call them blubs of the vestibule.” “Oh, their purpose is to squeeze the penis.” And then of course Freud separated out the “vaginal orgasm” from the “clitoral orgasm” with zero scientific evidence. It all seems to be part of this pattern of splitting up our bodies into disparate parts.
After doing this research, and talking a lot to Dr. Helen O’Connell, I took away that we were a lot more interconnected and whole than we were made out to be. The body parts we’re talking about all work together so intimately. They’re interconnected in their blood supply and their nerves, and in the sensations that they give us.
I liked [O’Connell’s] use of the word “clitoral complex” because it shows that all these tissues are intimately tied together in their fates, and physically incredibly close and touching. So there’s no such thing as an either/or framework here. There’s no, “Either you have this type of orgasm or this type of orgasm.” You can frame it that way: You can frame, like, a G-spot orgasm or a clitoral orgasm, but I think it does us a disservice. I personally appreciate having a more whole and interconnected view of my body. It feels less alienating to me than cordoning off different body parts and sexual experiences in the way that a lot of these male thinkers have done.
Cutchin: Biologists like Dr. Patty Brennan are mapping non-human genitalia and finding that animal vaginas are more “complex and variable” that anyone believed. Some details from Vagina Obscura made me laugh out loud. For example: that female dolphins masturbate by rubbing their clitorises against sand, other dolphins, and eels. Do you have a favorite animal genitalia?
Gross: I love koala vaginas! I was so blown away when I learned they have three vaginas. They have two on the outside and one that goes down the middle. The ones on the outside are where conception and insemination happen. And when they eject the joey into the pouch, that’s through the middle tube. Koalas can be pregnant always—pretty much forever. They often have a joey in the pouch, and then there’s another one gestating that will pop into the pouch as soon as the other one climbs onto their back. So koala mothers are often very fatigued. It takes quite a lot out of them.
The koala vagina illustrates what a beautiful multi-tasker the human vagina is. We’re doing it all—sex, reproduction, childbirth, protection against disease. Get you a tube that does it all.
Cutchin: Tell me about the “Father of Modern Gynecology,” James Marion Sims, a Southern slaveholder and doctor. When you say that the history of gynecology is intertwined with that of slavery, what do you mean?
Gross: You can’t separate the origins of modern gynecology from the history of slavery. Sims is credited with developing the vaginal speculum. He helped put American gynecology on the map globally. He also did his research on enslaved women, who we cannot say gave any form of true consent. They went through incredible pain and suffering at his hands.
Thanks to dogged historians, we now know the names of three of them: Lucy, Betsy and Anarcha. There’s been a really important effort to write them back into a history they were integrally a part of. In her book ‘Medical Bondage: Race, Gender, and the Origins of American Gynecology,’ Deirdre Cooper Owens showed that Lucy, Betsy and Anarcha were active participants in gynecology; they were serving as Sims’s surgical assistants. They were trained and working medically, and probably knew more about fistula [an abnormal opening between the vagina and bladder or rectum, which Sims was trying to treat] than any doctor at the time.
This history is important because so many advances in gynecology since then have come at the expense of vulnerable populations: the Tuskegee syphilis experiments [in which life-saving treatment was deliberately withheld from Black male subjects] and the contraception pill trials in Puerto Rico [in which women, who tended to be poor and lacking in education, were not adequately informed of potential side effects] are some of the most well-known, but there are so many more involving gray areas. Being aware that gynecology suffers from this history of ethical breeches should make scientists more cautious and thoughtful when they design experiments today.
Cutchin: If the medical establishment could take one or two lessons from Vagina Obscura, what do you hope they would be?
Gross: I don’t know that I wrote it for the medical establishment. I can make observations and see limitations as an outsider, but I didn’t write it as if I was going to give them a lesson. The takeaway for me was that patients are quite often experts in their own experience and their own reality. There’s a strong history of doctors not listening to them, or of trusting an outdated authority more than the people sitting in front of them.
But I do think there’s a broader lesson here for any researcher. There are so many fascinating avenues to explore and basic questions to answer, and we can only see these if we have different types of people asking questions. The book always comes back to this. It’s not only that more diversity equals better science, although that is also true. It’s that by shutting out whole groups of people from the enterprise of science—women and LBGT researchers, and patients, for example—we’ve missed fundamental questions and entire parts of the human body. That is such a huge loss, which is now finally being rectified. That’s really hopeful. But let’s try to do this more actively in the future.
‘Vagina Obscura’ Author Rachel E. Gross Takes Us on a Daring Anatomical Voyage. By Carli Cutchin. MS Magazine, April 26, 2022.
Patricia
Brennan never intended to become a champion of the vagina. Her journey, in
fact, began with a penis.
It was a late summer afternoon in 2000, and the 28-year-old Colombian biologist was stalking her study animal, a squat gray-blue bird called the great tinamou in the dense Costa Rican rainforest. As always, the forest floor was dark and shadowy, the sunlight swallowed up by the upper canopy. It was stiflingly humid; she was sweating through her protective gear. “You could die in that forest, and there would be no trace of you in just a few months,” she recalls. “You would disappear completely.”
That’s when she heard it: a pure, whistling tone, with an undertone of sadness. A male tinamou, calling for a mate. As she held her breath, a female appeared from the dense underbrush. She ran up to him, backed away, then chased him again. Finally she crouched down with her tail in the air, inviting him to mount. As Brennan watched through her binoculars, the male clambered clumsily onto her back. Brennan will never forget what happened next.
For most birds, mating is an artless affair. That’s because they don’t have external genitalia, just a multipurpose opening under the tail used to expel waste, lay eggs and have sex. (Biologists usually call this orifice a cloaca, which means “sewer” or “drain” in Latin. Brennan simply refers to it as the vagina, since it performs all the same functions and then some.) They briefly rub genitals together in an act known as a “cloacal kiss,” in which the male transfers sperm into the female. The whole event takes seconds.
But this time, the pair began waddling around, glued together. The male started thrusting. When he finally detached, she saw something dangling off him—something long, white and curly.
“What the hell is that thing?” she remembers thinking. “Oh, God, he’s got worms.”
Then she had another thought: “Man, is that a penis?”
Birds, she thought at the time, didn’t have penises. In her two years studying them at Cornell University, a world leader in avian research, she’d never once heard her colleagues mention a bird penis. And anyway, this certainly didn’t look like any penis she had ever seen—it was ghostly white, curled up like a corkscrew, thin as a piece of cooked spaghetti. Why would such an organ have evolved, only to have been lost in almost all birds? That would have been “the weirdest evolutionary thing,” she says.
When she returned to Cornell, she decided to learn everything there was to know about bird penises—which turned out to be not so much. Ninety-seven percent of all bird species have no phallus. Those that did, including ostriches, emus and kiwis, sported organs quite different from the mammalian variety. Corkscrew-shaped, they exploded out into the female in one burst, and engorged with lymphatic fluid rather than blood. Sperm traveled down spiraling grooves along the outside.
Brennan had been the first to observe a penetrative penis in this species of tinamou. Only later would she ask the question that would distinguish her from all her peers: If this was the penis, then what were the vaginas doing? “Obviously you can’t have something like that without some place to put it in,” she would later tell the New York Times. “You need a garage to park the car.” For the first time, she wondered about the size, shape, and function of that … er … garage.
In 2005, before she turned her lens to vaginas, the pursuit of penises led Brennan to the University of Sheffield in the English countryside. After realizing that “there is a huge gaping hole in our knowledge of this very fundamental part of bird biology,” she had pivoted her research and was now focusing on bird-penis evolution. She was here to learn the art of dissecting bird genitalia from Tim Birkhead, an evolutionary ornithologist. She got to work dissecting quail and finches, which had little in the way of outer genitalia. Next, she opened up a male duck from a nearby farm, and gasped.
The tinamou’s penis had been thin, like spaghetti. This one was thick and massive, but with the same recognizable spiral shape. Whoa, she thought. Wait a minute—where is this thing gonna go?
No one seemed to have an answer. The problem was, the typical bird-dissection technique focused almost entirely on the male. When researchers did dissect a female duck, they sliced all the way up through the sides of the vagina to get at the sperm-storage tubules near the uterus (in birds, it’s called the shell gland), distorting their true anatomy. They tossed the rest out, unexamined. When she asked Birkhead what the inside of a female duck’s reproductive tract looked like, she recalls, he assumed it was the same as any other bird: a simple tube.
But she knew there was no way an appendage as complex and unusual as the duck penis would have evolved on its own. If the penis were a long corkscrew, the vagina ought to be an equally complex structure.
The first step was to find some female ducks. Brennan and her husband drove out to one of the surrounding farms and purchased two Pekin ducks, which she euthanized without ceremony on a bale of hay. (Brennan’s husband is used to these kind of excursions: “He brings me roadkill as a nuptial gift,” she says.) Instead of slicing the reproductive tract up the sides, she spent hours carefully peeling away the tissues, layer by layer, “like unwrapping a present.” Eventually, a complex shape emerged: twisted and mazelike, with blind alleys and hidden compartments.
When she showed Birkhead, they both did a double-take. He had never seen anything like it. He called a colleague in France, a world expert on duck reproductive anatomy, and asked him if he’d ever heard of these structures. He hadn’t. The colleague went to examine one of his own female specimens, and reported back the same thing: an “extraordinary vagina.”
It was a late summer afternoon in 2000, and the 28-year-old Colombian biologist was stalking her study animal, a squat gray-blue bird called the great tinamou in the dense Costa Rican rainforest. As always, the forest floor was dark and shadowy, the sunlight swallowed up by the upper canopy. It was stiflingly humid; she was sweating through her protective gear. “You could die in that forest, and there would be no trace of you in just a few months,” she recalls. “You would disappear completely.”
That’s when she heard it: a pure, whistling tone, with an undertone of sadness. A male tinamou, calling for a mate. As she held her breath, a female appeared from the dense underbrush. She ran up to him, backed away, then chased him again. Finally she crouched down with her tail in the air, inviting him to mount. As Brennan watched through her binoculars, the male clambered clumsily onto her back. Brennan will never forget what happened next.
For most birds, mating is an artless affair. That’s because they don’t have external genitalia, just a multipurpose opening under the tail used to expel waste, lay eggs and have sex. (Biologists usually call this orifice a cloaca, which means “sewer” or “drain” in Latin. Brennan simply refers to it as the vagina, since it performs all the same functions and then some.) They briefly rub genitals together in an act known as a “cloacal kiss,” in which the male transfers sperm into the female. The whole event takes seconds.
But this time, the pair began waddling around, glued together. The male started thrusting. When he finally detached, she saw something dangling off him—something long, white and curly.
“What the hell is that thing?” she remembers thinking. “Oh, God, he’s got worms.”
Then she had another thought: “Man, is that a penis?”
Birds, she thought at the time, didn’t have penises. In her two years studying them at Cornell University, a world leader in avian research, she’d never once heard her colleagues mention a bird penis. And anyway, this certainly didn’t look like any penis she had ever seen—it was ghostly white, curled up like a corkscrew, thin as a piece of cooked spaghetti. Why would such an organ have evolved, only to have been lost in almost all birds? That would have been “the weirdest evolutionary thing,” she says.
When she returned to Cornell, she decided to learn everything there was to know about bird penises—which turned out to be not so much. Ninety-seven percent of all bird species have no phallus. Those that did, including ostriches, emus and kiwis, sported organs quite different from the mammalian variety. Corkscrew-shaped, they exploded out into the female in one burst, and engorged with lymphatic fluid rather than blood. Sperm traveled down spiraling grooves along the outside.
Brennan had been the first to observe a penetrative penis in this species of tinamou. Only later would she ask the question that would distinguish her from all her peers: If this was the penis, then what were the vaginas doing? “Obviously you can’t have something like that without some place to put it in,” she would later tell the New York Times. “You need a garage to park the car.” For the first time, she wondered about the size, shape, and function of that … er … garage.
In 2005, before she turned her lens to vaginas, the pursuit of penises led Brennan to the University of Sheffield in the English countryside. After realizing that “there is a huge gaping hole in our knowledge of this very fundamental part of bird biology,” she had pivoted her research and was now focusing on bird-penis evolution. She was here to learn the art of dissecting bird genitalia from Tim Birkhead, an evolutionary ornithologist. She got to work dissecting quail and finches, which had little in the way of outer genitalia. Next, she opened up a male duck from a nearby farm, and gasped.
The tinamou’s penis had been thin, like spaghetti. This one was thick and massive, but with the same recognizable spiral shape. Whoa, she thought. Wait a minute—where is this thing gonna go?
No one seemed to have an answer. The problem was, the typical bird-dissection technique focused almost entirely on the male. When researchers did dissect a female duck, they sliced all the way up through the sides of the vagina to get at the sperm-storage tubules near the uterus (in birds, it’s called the shell gland), distorting their true anatomy. They tossed the rest out, unexamined. When she asked Birkhead what the inside of a female duck’s reproductive tract looked like, she recalls, he assumed it was the same as any other bird: a simple tube.
But she knew there was no way an appendage as complex and unusual as the duck penis would have evolved on its own. If the penis were a long corkscrew, the vagina ought to be an equally complex structure.
The first step was to find some female ducks. Brennan and her husband drove out to one of the surrounding farms and purchased two Pekin ducks, which she euthanized without ceremony on a bale of hay. (Brennan’s husband is used to these kind of excursions: “He brings me roadkill as a nuptial gift,” she says.) Instead of slicing the reproductive tract up the sides, she spent hours carefully peeling away the tissues, layer by layer, “like unwrapping a present.” Eventually, a complex shape emerged: twisted and mazelike, with blind alleys and hidden compartments.
When she showed Birkhead, they both did a double-take. He had never seen anything like it. He called a colleague in France, a world expert on duck reproductive anatomy, and asked him if he’d ever heard of these structures. He hadn’t. The colleague went to examine one of his own female specimens, and reported back the same thing: an “extraordinary vagina.”
To Brennan, it seemed that females were responding in some way to males, and vice versa. But there was something odd going on: the vagina twisted in the opposite direction of the male’s. In other words, this vagina seemed to have evolved not to accommodate the penis, but to evade it. “I couldn’t wrap my head around it. I just couldn’t,” Brennan says. She preserved the structures in jars of formaldehyde and spent days turning them over, trying to figure out what could explain their complexity.
That’s when she began thinking about conflict. Duck sex, she knew, could be notoriously violent. Ducks tended to mate for at least a season. However, extra males lurked in the wings, ready to harass and mount any paired female they could get their hands on. This often leads to a violent struggle, in which males injure or even drown the female. In some species, up to 40 percent of all matings are forced. The tension is thought to stem from the two sexes’ competing goals: The male duck wants to sire as many offspring as possible, while the female duck wants to choose the father of her children.
This story of conflict, Brennan suspected, might also shape duck genitalia. “That was the part where I was like: holy cow,” she says. “If that’s really going on, this is nuts.” She started contacting scientists across North and South America to collect more specimens. One was Kevin McCracken, a geneticist at the University of Alaska who, while out on a wintry jaunt, had discovered the longest known bird phallus on the Argentine lake duck, which unraveled to a stunning 17 inches. He suggested that perhaps the male was responding to female preference—wink-wink, nudge-nudge—but hadn’t bothered to actually examine the female.
When Brennan called him up, he was more than happy to help her collect more specimens. Today, he admits that perhaps the reason he hadn’t considered looking at the female side of things was a result of his own male bias. “It was fitting that a woman followed this up,” he says. “We didn’t need a man to do it.”
By carefully dissecting the genitals of 16 species of waterfowl, Brennan and her colleagues found that ducks showed unparalleled vaginal diversity compared to any known bird group. There was a lot going on inside those vaginas. The main purpose, it appeared, was to make the male’s job harder: It was like a medieval chastity belt, built to thwart the male’s explosive aim. In some cases, the female genital tract prevented the penis from fully inflating, and was full of pockets where sperm went to die. In others, muscles surrounding the cloaca could block an unwanted male, or dilate to allow entry to a preferred suitor.
Whatever the females were doing, they were succeeding. In ducks, only 2 to 5 percent of offspring are the result of forced encounters. The more aggressive and better endowed the male, the longer and more complex the female reproductive tract became to evade it. “When you dissected one of the birds, it was really easy to predict what the other sex was going to look like,” Brennan told the New York Times. It was a struggle for reproductive control, not bodily autonomy: Although a female couldn’t avoid physical harm, her anatomy could help her gain control over the genes of her offspring after a forced mating.
The duck vagina, Brennan realized, was hardly the passive, simple structure that biologists had made it out to be. In fact, it was an expertly rigged penis-rejection machine. But what about in other animal groups?
A world opened up before Brennan’s eyes: the vast variety of animal vaginas, wonderfully varied and woefully unexplored. For centuries, biologists had praised the penis, fawning over its length, girth, and weaponry. Brennan’s contribution, simple as it may seem, was to look at both halves of the genital equation. Vaginas, she would learn, were far more complex and variable than anyone thought. Often, they play active roles in deciding whether to allow intruders in, what to do with sperm, and whether to help a male along in his quest to inseminate. The vagina is a remarkable organ in its own right, “full of glands and full of muscles and collagen, and changing constantly and fighting pathogens all the time,” she says. “It’s just a really amazing structure.”
To center females in genitalia studies, she knew she would need to go beyond ducks and start to open “the copulatory black box” of female genitalia more broadly. And, as she explored genitals, from the tiny, two-pronged snake penis to the spiraling bat vagina, she kept finding the same story: Males and females seemed to be co-evolving in a sexual arms race, resulting in elaborate sexual organs on both sides.
But conflict, it turned out, was hardly the only force shaping genitals.
For decades, biologists had noted a strange feature found in the reproductive tracts of marine mammals like dolphins, whales and porpoises: a series of fleshy lids, like a stack of funnels, leading up to the cervix. In the literature, they were known as “vaginal folds,” and were thought to have evolved to keep sperm-killing seawater out of the uterus. But to Dara Orbach, a Canadian PhD student who was studying the sexual anatomy of dolphins, that function didn’t explain the variation she was finding. After a chance pairing brought her together with Brennan in 2015, she brought her collection of frozen vaginas to Brennan’s lab to investigate.
What they found at first reminded them strongly of the duck story. In the harbor porpoise, for instance, the vagina spiraled like a corkscrew and had several folds blocking the path to the cervix. Porpoise penises, in turn, ended in a fleshy projection, like a finger, that seemed to have evolved to poke through the folds and reach the cervix. Just as in ducks, it seemed that males and females were both evolving specialized features in order to gain the evolutionary advantage during sex.
Then, in the middle of their dolphin vagina dissections, the scientists stumbled across something else: a massive clitoris, partly enfolded in a wrinkled hood of skin. While the human clitoris has long been cast (erroneously) as small and hard to find, this one was virtually impossible to miss. When fully dissected out, it was larger than a tennis ball. “It was enormous,” Brennan says.
That dolphins would have a well-developed clitoris was no surprise. Brennan and Orbach both knew that these charismatic creatures engage in frequent sexual behavior for reasons like pleasure and social bonding. Females have been seen masturbating by rubbing their clitorises against sand, other dolphins’ snouts and objects on the sea floor. Yet while other scientists had guessed that the dolphin clitoris might be functional, no one had actually tried to figure out how it worked.
By dissecting 11 dolphin clitorises and running the samples through a micro CT scanner, the researchers uncovered a roughly triangular complex of tissues that sat just at the opening of the vagina—easily accessible to a penis, snout or fin. It was made up of two types of erectile tissue, both spongy and porous, allowing it to swell with arousal. These erectile bodies also grew and changed shape during puberty, suggesting they played an important role during adult sexual life. Strikingly large nerves, up to half a millimeter in diameter, ended in a web of sensitive nerve endings just beneath the skin.
In short, the dolphin clitoris looked a whole lot like the human clitoris, they reported in a paper published in January. And it probably worked like one, too. Brennan can’t say for certain that dolphins have orgasms, “But I’m pretty darn sure that sex feels good to them. Or at least that rubbing of the clitoris feels good,” she says.
Before dolphins, even Brennan had not given much thought to role that non-reproductive sexual behavior might play in the evolution of genitals. In general, she subscribed to the tenets of classic Darwinian evolutionary thinking: “In my mind, everything ultimately has got to be reproductive,” she says. Perhaps, she thought, these behaviors might encourage future reproductive sex, eventually leading to more offspring. Or, a male’s ability to stimulate the clitoris might influence a female’s choice of mate.
Yet when it came to genital evolution, Darwin left much to be desired. The father of evolution generally eschewed talking about genitals, considering their main function to be fitting together mechanically, as a lock fits into a key. Moreover, he characterized female animals almost universally as chaste, modest and virtually devoid of sexual urges. In his lesser known writings, he described a world in which females honored their “husbands” and kept “marriage-vows.” Although he observed a few counter-examples—i.e. females with several “husbands” or those that seemed to pursue sex for pleasure—he steered clear of them, likely out of a sense of Victorian propriety.
To Darwin, males were the ones with the driving urge to engage in sexual behavior. The role of females, by contrast, was primarily to choose between competing males. “The males are almost always the wooers; and they alone are armed with special weapons for fighting with their rivals,” he wrote in his 1871 book Descent of Man, and Selection in Relation to Sex. "They are generally stronger and larger than the females, and are endowed with the requisite qualities of courage and pugnacity.”
A century and a half later, Darwin’s influence still casts a long shadow over the field. In her frank exploration of animal vaginas, Brennan is beginning to challenge some the traces of prudery, male bias and lack of curiosity about female genitals that Darwin left behind. Yet she too had inherited some of that framework: Namely, she still thought about genitals mainly in conjunction with reproductive, heterosexual sex.
What she found in dolphins gave her pause. The substantial clitoris before her was a hint at something that seems obvious, but often isn’t: sex isn’t just for reproduction.
Today, we know that genitalia do far more than just fit together mechanically. They can also signal, symbolize and titillate—not just to a potential mate, but to other members of a group. In humans, dolphins and beyond, sexual behavior can be used to strengthen friendships and alliances, make gestures of dominance and submission, and as part of social negotiations like reconciliation and peacemaking, points out evolutionary biologist Joan Roughgarden, author of the 2004 book Evolution’s Rainbow: Diversity, Gender, and Sexuality in Nature and People.
These other uses of sex may be one reason that animal genitalia are so weird and wonderful beyond your standard vagina/penis combo. Consider the long, pendulous clitorises that dangle from female spider monkeys and are used to distribute scent; the notorious hyena clitoris, which is the same size as the male’s penis and used to urinate, copulate and give birth; and the showstopping genitalia that Darwin did briefly highlight in monkeys—the rainbow-hued genitals of vervets, drills and mandrills, and the red swellings of female macaques in estrus—that may connote social status and help troupes avoid conflict.
These diverse examples of “genital geometry” (Roughgarden’s term) serve a multitude of purposes beyond reproduction. “All our organs are multifunctional,” she points out. “Why shouldn’t the genitals be as well?”
Across the animal kingdom, same-sex behavior is widespread. In female-dominated species like bonobos, for instance, same-sex matings are at least as common as between-sex matings. Notably, female bonobos have massive, cantaloupe-sized labial swellings and prominent clitorises that can reach two and a half inches when erect. Some primatologists have gone so far as to suggest that the position of this remarkable clitoris—it’s in a frontal position, as in humans, and unlike in pigs and sheep, which have clitorises inside their vaginas—might have developed to facilitate same-sex genital rubbing.
“It does seem more logistically favorable, let’s say, for the kinds of sex they’re having,” says primatologist Amy Parish, a bonobo expert who was the first to describe bonobo societies as matriarchal. Primatologist Frans de Waal, too, has mused that “the frontal orientation of the bonobo vulva and clitoris strongly suggest that the female genitalia are adapted for this position.” Roughgarden has therefore coined this clitoral configuration the “Mark of Sappho.” And given that bonobos, like chimps, are some of our closest evolutionary cousins—they share 98.5 percent of our genes—she wonders why more scientists haven’t asked whether the same forces could be at play in humans.
These are questions that the current framework of sexual selection, with its simple assumptions about aggressive males and choosy females, renders unaskable. Darwin took for granted that the basic unit of nature was the female-male pairing, and that such pairings always led to reproduction. Therefore, the theory he came up with—coy females who pick among competing males—only explained a limited slice of sexual behavior. Those who followed in his footsteps similarly treated heterosexuality as the One True Sexuality, with all other configurations as either curiosities or exceptions.
The effects of this pigeonholing go beyond biology. The dismissal of homosexuality in animals, and the treatment of such animals as freaks or exceptions, helps reify negative attitudes toward sexual minorities in humans. Darwin’s theories are often misused today to promote myths about what human nature should and shouldn’t be. Roughgarden, a transgender woman who transitioned a few years before writing her book, could see the damage more clearly than most. Sexual selection theory “denies me my place in nature, squeezes me into a stereotype I can’t possibly live with—I’ve tried,” she writes in Evolution’s Rainbow.
Focusing solely on a few dramatic cases of sexual conflict—the “battle of the sexes” approach—obscures some of the other powerful forces that shape genitals. Doing so risks leaving out species in which the sexes cooperate and negotiate, including monogamous seabirds like albatrosses and penguins, and those in which homosexual bonds are as strong as heterosexual ones. In fact, it appears that the stunning variety of animal genitals are shaped by an equally stunning variety of driving forces: conflict, communication, and the pursuit of pleasure, to name a few.
And that, to both Brennan and Roughgarden, is freeing. “Biology need not limit our potential. Nature offers a smorgasbord of possibilities for how to live,” Roughgarden writes. Rather than chaste Victorian couples marching two by two up the ramp into Noah’s neat and tidy ark, “the living world is made of rainbows within rainbows within rainbows, in an endless progression.”
Adapted from Vagina Obscura: An Anatomical Voyage. By Rachel E. Gross. W. W. Norton & Company, 2022.
Why Have Female Animals Evolved Such Wild Genitals? By Rachel E. Gross. Smithsonian Magazine, March 31, 2022.
Your vagina is a mystery, an enigma, a world that has been largely uncharted, underestimated and misunderstood since the start of humankind. It holds more secrets than the Sphinx and can seem more distant than Mars, more unfamiliar than the ocean floor. Because, until recent decades — when people with vaginas have made painstaking headway into the realms of science and health — the pursuit of such knowledge has been left to men. To put it lightly, they blew it.
As Rachel E. Gross proves in “Vagina Obscura,” the impact of this neglect cannot be overstated. Taking readers on an expansive journey across continents, cultures, centuries and even species, Gross reveals a stunning disparity in Western medicine and academia: While huge amounts of money and dedication are poured into the understanding of penises, the female body is disregarded. Like lore, this misinformation and shame are still being passed down to girls today.
Gross experienced this “knowledge gap” firsthand at 29, when she was prescribed what was “basically rat poison” to treat a bacterial infection in her vagina. It was then that she realized “I knew almost nothing about how my vagina worked” — and that no one else really does either.
She cites Darwin’s journal entry declaring that a woman’s purpose was to be “a nice soft wife,” “an object to be beloved and played with. Better than a dog anyhow.” Freud, who admitted he knew little about womankind (that “little creature without a penis”), would influence gynecology through the 20th century, and even today.
Not until 1993 did a federal mandate require that “women and minorities” be included in clinical trials. Only in 2014 did the National Institutes of Health start a branch to study vulvas, vaginas, ovaries and uteruses. And in 2009, the bioengineer Linda Griffith opened America’s first and only lab (at M.I.T.) to research endometriosis. “My niece who’s 16 was just diagnosed,” Griffith says in the book. “And there’s no better treatment for her — 30 years younger than me — than there was for me when I was 16.”
In the 1980s, medical textbooks called endometriosis “the career woman’s disease” — language that had been recirculated for generations. A century earlier, coinciding with first-wave feminism in Europe, doctors — buttressed by Freud’s 1895 “Studies on Hysteria” — suggested that higher education and careers “might siphon blood from their uteruses to their brains.” In the 1870s, higher education was thought to “shrivel a woman’s ovaries and keep her from her motherly duties.”
Of course, the word “hysteria” — derived from the Greek hystera, or womb — has been used to degrade women for centuries, as one of the first mental health conditions attributed only to them. Gross adds to this history the recent argument that hysteria was endometriosis all along. If true, “this would constitute one of the most colossal mass misdiagnoses in human history,” according to a 2012 paper by Iranian endometriosis surgeons, one that “has subjected women to murder, madhouses and lives of unremitting physical, social and psychological pain.”
Gross takes on a herculean task, exploring female anatomy from a medical, social and historical perspective, in eight chapters ranging in topic from the glans clitoris to the egg cell to the vaginal microbiome. Some passages skew medically dense and might be wince-inducing for the squeamish. But Gross manages to make palatable the sawing of cadavers and the injecting of silicone into two-pronged snake vaginas, without undercutting the gravity of their resulting revelations.
She achieves this by way of personal stories, like those of Miriam Menkin, the first researcher to fertilize a human egg outside the body; the OB-GYN Ghada Hatem, who performs clitoral restoration surgery on women who have endured genital cutting; Aminata Soumare, a young Frenchwoman whose clitoris was excised when she was a baby in Mali; and the gynecologist Marci Bowers, who has elevated gender-affirming surgery to an art form, prioritizing the construction of a functioning, sensitive clitoris.
And it is no wonder that the clitoris has been “demonized, dismissed and left to the trash heap of history.” An organ that exists almost entirely beneath the body’s surface, it was termed “membre honteux,” or “the shameful member,” by a French anatomist in 1545. Because, extraordinarily, it is the only human organ whose primary function is pleasure.
Vagina Obscura : an Anatomical Voyage. By Rachel E. Gross
Illustrated. 307 pp. W.W. Norton & Company. $30.
‘Vagina Obscura’ Demystifies Female Anatomy. By Maya Salam. The New York Times, March 29, 2022.
Page on the website of W.W. Norton, publisher of the book
More
reviews of Vagina Obscura, page on the website of the author
Page on the website of the author about her book












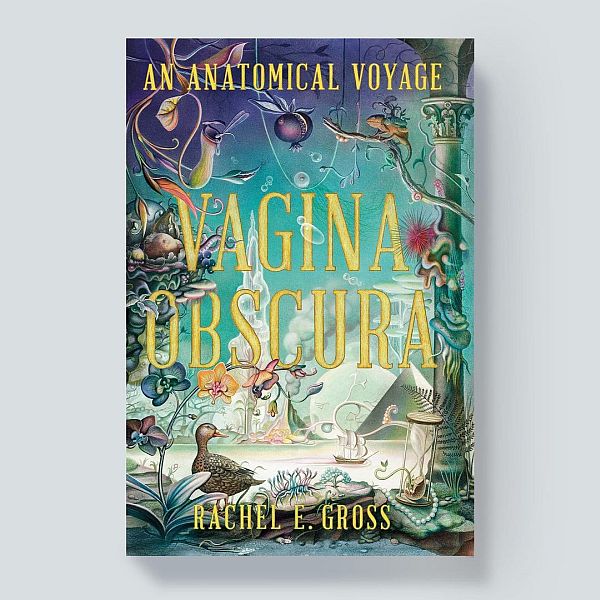
No comments:
Post a Comment